what are the long-term side effects of gallbladder removal? Does gallbladder removal have side effects? Here is a study on the effects of gallbladder removal and what you should do instead.
A Gallbladder surgery, also known as a Cholecystectomy (CCY) is one of the most commonly performed surgeries. This surgery is performed when someone has gallbladder stones with pain/tenderness on the right side of the abdomen after eating any oily or fatty foods.
If a person is told their gallbladder is loaded with stones, then they have had a digestion problem for many years prior.
And chances are there is more within their digestive system that is imbalanced than their gallbladder. Of course, if there is a life-threatening emergency and the only way to save your life is to remove the GB then you should go for it.
It is also one of the most unnecessary and avoidable surgeries. There is a better way! So, what are the long-term side effects of gallbladder removal? Well, read on to find out why you should avoid removing your gallbladder.
Long-Term Effects Of Gallbladder Removal
According to the Journal of Gastroenterology, the long-term consequences of removing an organ that helps you process fats can leave you with any of the following lifelong symptoms:
- Almost immediate diarrhea with oils or fat consumption
- Nausea or vomiting with fat consumption
- Metabolic consequences of unstable blood sugar and altered insulin production. The American Journal of Gastrointestinal Liver Physiology found those with a CCY had deterioration of normal blood sugar after meals. Optimizing bile acids and thinning out the sludge of the gallbladder is essential for stabilizing blood sugar. I find people who have hypoglycemia, diabetes, or dysglycemia can have fat digestion issues.
- Poor absorption of amino acids, low albumin. White spots on the nails or ridges can indicate poor absorption of amino acids and minerals. This is usually from low stomach acid but could signal there is a broader digestive issue too.
- Prolonged iron anemia. There are many reasons for iron anemia, but this is another interesting association.
- Higher risk for colon dysplasia – abnormal growth of cells, polyps which can be pre-cancerous or cancerous.
There is a particular set of people who should not get their gallbladder taken out. According to The Journal of Gastroenterology those with Crohn’s Disease (CD) who had their GB taken out had:
- Higher disease activity
- More years with iron anemia
- Chronic abdominal pain
- Lower protein absorption
- Worse quality of life
- More hospital admissions
- Higher risk for colonic dysplasia
- Higher opioid use
I have helped save many patients from having their gallbladder taken out. This is done with a gallbladder cleanse (and they send us pictures of the stones!)
You should only do this with the supervision of your functional medicine practitioner, who has experience guiding people with doing a Gallbladder Cleanse.
Each person’s duration is specific to how poor their fat digestion may be, and labs are drawn to make sure it is done safely.
A Liver and Gallbladder Cleanse is not recommended for women who are pregnant or nursing. Do not proceed with this cleanse if you are feeling ill, have a fever, cold-like symptoms, or have not had a bowel movement in a few days.
When gallbladder stones are released, they are often light green or dark green. A GB cleanse can be done every 6 weeks and the more often they are done, the color of the stones will change.
How Can You Tell If You Have Gallbladder Stasis or Stones?
- Pain or tenderness on the right side under the rib cage after eating any oily or fatty foods.
- Diarrhea or loose stools with eating too much fat
- Nausea or vomiting if you eat too much fat
- Clay-colored stools that can sometimes have mucus around it
- Floating stools
- Blood work shows elevated LDH, GGT, AST, Alk Phos
- Stool testing can see what percentage of the stool contains fat, which may allude to a gallbladder issue.
More Helpful Blog Posts For You
- Travel Insurance I & II 60c: Travel without the threat of mosquito, parasite, and bacterial infections
- PROVEN Alternative Ways To Eradicate H. Pylori
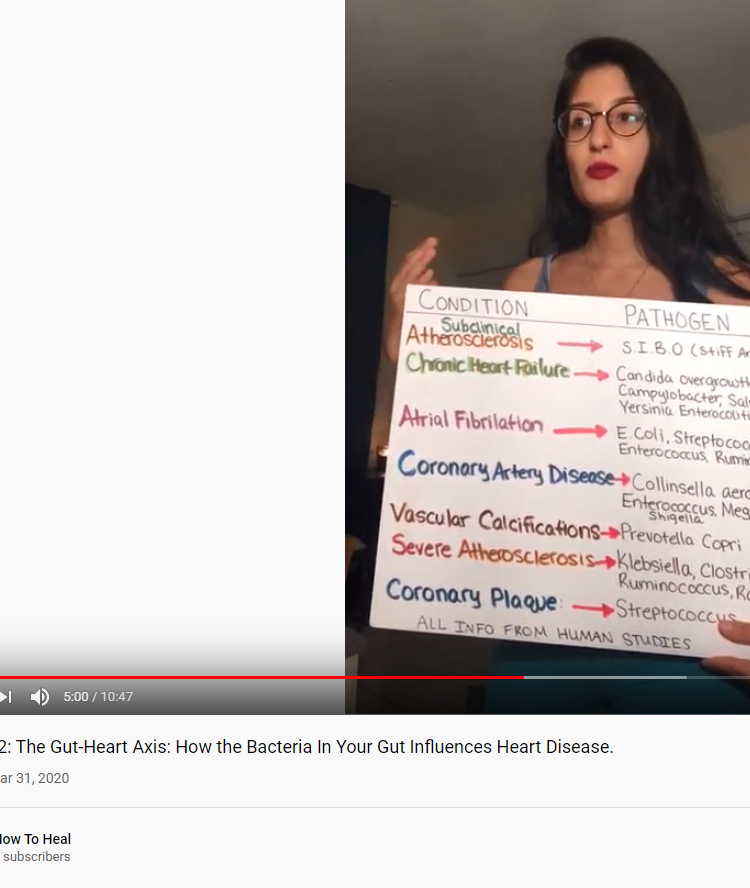
- How Our Gut Bacteria Influences Various Heart Diseases & Risk Factors
- A Deficiency In This Fatty Acid Can Be Causing Your Diabetes, Depression, Weight Gain, & Neurodegen. Diseases
- Probiotics Improve Major Depressive Disorder
Sources: